A pacemaker is a small device that’s placed in your chest to help control arrhythmias (irregular heart rhythms). This device is especially helpful if you have a slow heart rate.
Pacemakers use low-energy electrical pulses to correct faulty electrical signaling in your heart that can be dangerous. These devices can also help restore a normal heart rate, allowing you to be more active again.
Valley’s electrophysiologists are experts in using pacemakers to help you feel better and reduce serious health risks.
Am I a Candidate for a Pacemaker?
A pacemaker may be right for you if you have one of the following:
- A heartbeat that is too slow (bradycardia)
- A heartbeat that is too fast (tachycardia) because of atrial fibrillation (AFib) or another cause
- Heart failure
- Disease of the heart muscle (cardiomyopathy)
- Heart defects that you’ve had since birth (congenital heart defects)
- Previous heart attack, heart surgery or heart transplant
Benefits of a Pacemaker
A pacemaker can reduce arrhythmia symptoms such as:
- Fainting (syncope)
- Fatigue
- Shortness of breath
- Dizziness
- Pounding in your chest (palpitations)
If you have these issues or symptoms, Valley’s electrophysiologists can help you decide if a pacemaker is right for you.
Types of Pacemakers
Valley offers the most advanced types of pacemakers. Some work all the time to control your heart rhythm, while others act as “backup” when needed.
Which pacemaker is right for you depends on the type of arrhythmia you have. Our electrophysiologists will work with you to determine the best option for you.
Single Chamber Pacemaker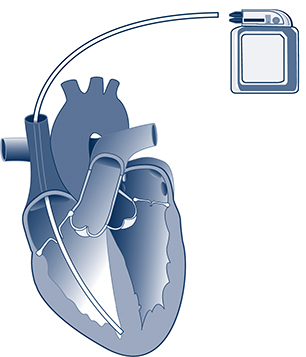
Your electrophysiologist may use a single chamber pacemaker (shown at right) if you have chronic atrial fibrillation (AFib). This device contains one lead (wire) that is usually threaded to the ventricle, the lower chamber of the heart.
Dual Chamber Pacemaker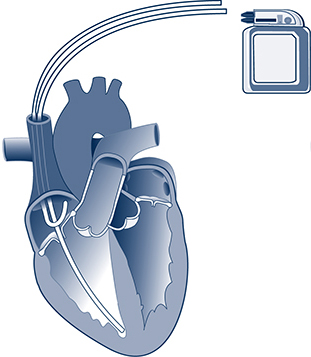
A dual chamber pacemaker (shown at right) is used to bring the upper and lower chambers of your heart in sync. This device can also help if your heart’s electrical signal is blocked (heart block or AV block).
A dual chamber pacemaker has two wires. One is threaded to your heart’s upper chamber, the atrium. The other is threaded to its lower chamber, the ventricle.
Biventricular Pacemaker (CRT-P)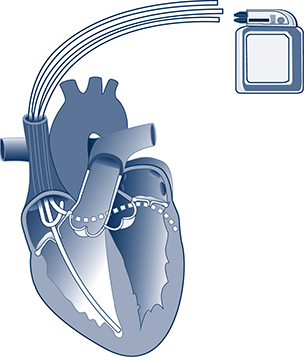
Your electrophysiologist may use a biventricular pacemaker (shown at right) if you have heart failure or decreased heart function. This type of pacemaker is also called a cardiac resynchronization therapy pacemaker (CRT-P).
Leadless Pacemaker
This latest type of pacemaker (shown at right) works in the lower chamber on the right side of your heart. It does the same job as a single chamber pacemaker but without wires.
A leadless pacemaker is shaped like a AA battery. Your electrophysiologist may recommend this device if you do not experience symptoms every day.
What Happens During Pacemaker Implant Surgery?
The procedure is different if you are having a pacemaker with leads or a leadless pacemaker.
If You Get a Pacemaker with Leads
Here’s what you can expect if you are having surgery for a pacemaker with leads:
- Ask someone to drive you to and from the hospital on the day of your procedure. You’ll need someone to drive you home after the procedure.
- At Valley, a nurse will start an intravenous (IV) line with an antibiotic to prevent infection.
- A nurse will shave and clean one side of your chest.
- Your team will include your electrophysiologist, interventional cardiologist, anesthesiologist and other experts.
- Your anesthesiologist will give you local anesthesia to numb the area of the incisions. They will also give you medicine through the IV to help you relax and sleep.
- Your electrophysiologist or interventional cardiologist will make a small incision below your collarbone to reach a vein leading to your heart.
- They will thread one or more flexible wires (leads) through that vein into the heart using X-ray guidance.
- They will attach one end of each wire in your heart. They will attach the other end to the pacemaker, which is usually implanted under the skin beneath your collarbone.
- The surgery takes about one to three hours.
If You Get a Leadless Pacemaker
Here’s what you can expect if you are having surgery for a leadless pacemaker:
- Ask someone to drive you to and from the hospital on the day of your procedure. You’ll need someone to drive you home after the procedure.
- At Valley, a nurse will start an intravenous (IV) line with an antibiotic to prevent infection.
- A nurse will shave and clean one side of your chest.
- Your team will include your electrophysiologist, interventional cardiologist, anesthesiologist and other experts.
- Your anesthesiologist will give you local anesthesia to numb the area of the incisions. They will also give you medicine through the IV to help you relax and sleep.
- Your electrophysiologist or interventional cardiologist will make a small incision into your groin to reach a vein leading to your heart.
- They will move the leadless pacemaker through that vein into the heart using X-ray guidance.
- They will attach the leadless pacemaker to the wall of your heart.
- The surgery usually takes one to three hours.
Recovery After Your Pacemaker Procedure
Here’s what you can expect immediately after your pacemaker procedure:
- You’ll usually stay in the hospital overnight and go home the following day.
- Before you go home, your doctor will program your pacemaker to fit your specific needs.
Here’s what to expect when you go home:
- You may be sore where your pacemaker was implanted. Over-the-counter acetaminophen and ice can help ease pain.
- Avoid taking aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or diclofenac. These can cause bleeding.
- Your electrophysiologist may recommend that you avoid bathing and driving for a week after your procedure.
- Your electrophysiologist may recommend avoiding heavy lifting and vigorous exercise for about a month. They may also suggest not lifting your arm above your shoulder for a month.
- You’ll return to your electrophysiologist’s office in seven to 10 days so the team can check you and your device.
- After that, most pacemakers can be checked remotely using wireless technology. Your pacemaker will send information on your heart rhythm to our office remotely. This saves you from making trips to the office.
Call your electrophysiologist if you have:
- Bleeding
- Discharge (pus) or swelling near the incision
- Chest pain
- Shortness of breath
- Dizziness
- Fainting or near-fainting
- Fever
- Chills
Lead Extraction for a Pacemaker
If you have a pacemaker with leads, you have wires inside your heart connected to your device. Some people may need to have their leads removed because of damage, infection or other reasons.
At Valley, our electrophysiology team is highly skilled at performing lead extractions. They can also replace old leads with new leads so you can continue your treatment.
Why Choose Valley for a Pacemaker?
- Collaborative approach to pacemaker placement: Our electrophysiologists and interventional cardiologists work together during your pacemaker procedure to ensure the best outcomes. Our team will work closely with you before, during and after your procedure.
- The latest pacing techniques: Our electrophysiologists use advanced techniques with pacemakers that are not available at many centers. These techniques involve placing the wires in different locations of the heart to get its contractions in sync. Patients who have these pacing techniques often feel better and have better outcomes.
- Remote monitoring from your home: Your Valley care team will regularly monitor the data sent wirelessly from your pacemaker. This helps you avoid unnecessary trips to the clinic when your heart rhythm is under control.
- Pacemaker and AFib expertise: Valley’s Snyder Center for Comprehensive Atrial Fibrillation offers pacemakers and other innovative ways to treat and manage AFib and other arrhythmias. Our electrophysiologists also lead clinical trials to test treatments for a range of heart rhythm conditions.