You might feel like your heart is “skipping a beat” sometimes, which can be a sign of an arrhythmia (abnormal heart rhythm), but it’s important to remember that most arrhythmias are harmless.
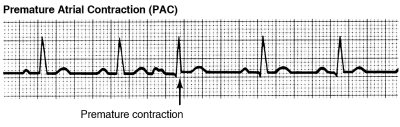
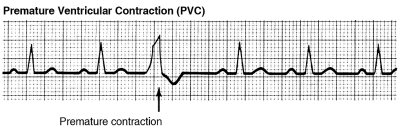
Both Premature Atrial Contractions (PACs) and Premature Ventricular Contractions (PVCs) are early, extra heartbeats – most benign arrhythmias are these types, and don’t require that you have any treatment.
If you experience lots of PACs or PVCs, however, or have symptoms associated with them, that’s a sign that it’s time to be evaluated by a cardiologist, who may send you to a member of our group here at Valley.
Of course, some types of arrhythmia, are clinically significant. If we suspect that’s the case, we’ll work with you to personalize a treatment plan, beginning with tests specifically tailored to your situation.
Tachycardia / Tachyarrhythmia
Tachycardia is a very fast heartbeat, over 100 beats per minute. During exercise, the heart rate also goes up naturally. However, when tachycardia is an abnormal state, we call it tachyarrhythmia and must address it with you through further testing and treatment. Below, we discuss various types of tachyarrhythmias:

Supraventricular Arrhythmias
These arrhythmias begin in the atria, and are usually not life-threatening. Supraventricular arrhythmias can be an inconvenience because of their symptoms (chest pain, dizziness, pounding pulse, etc.), but can be treated with medication or catheter ablation which type of treatment you have will be decided after we work with you to evaluate your case.
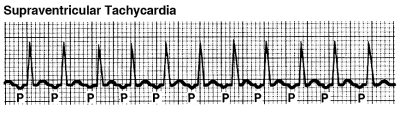
Types of supraventricular arrhythmias include:
- Paroxysmal Supraventricular Tachycardias (PSVTs) – Occasional episodes of very rapid but regular heartbeat that come from the atria. These episodes start and stop suddenly
- AV Nodal Re-entrant Tachycardia (AVNRT) – This is the most common type of rapid heartbeat, occurring in 60-65% of cases, and is caused by the presence of more than one pathway in the heart. There are two pathways leading into the atrioventricular (AV) node – one fast (which is customarily used to conduct the normal electrical impulses in the heart) and one slow. The extra beats find the fast pathway already in use, so they use the slow pathway, causing a “short circuit.”
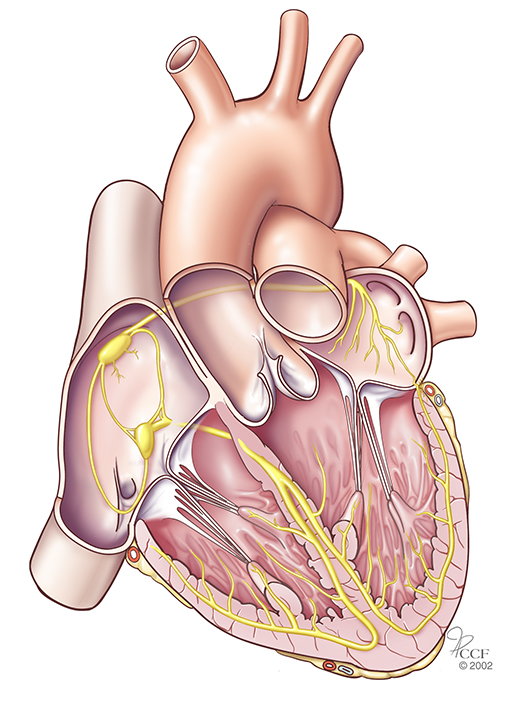 AV Re-entrant Tachycardia (aka Bypass Tract Tachycardias) – This type of rapid heart rhythm comprises 30-35% of paroxysmal tachycardia cases, and is caused by an extra conduction pathway in the heart, which is triggered by an extra beat. The condition involves ventricles as well as atria, and the beat is going through an extra abnormal connection, also known as an accessory pathway (see image at right).
AV Re-entrant Tachycardia (aka Bypass Tract Tachycardias) – This type of rapid heart rhythm comprises 30-35% of paroxysmal tachycardia cases, and is caused by an extra conduction pathway in the heart, which is triggered by an extra beat. The condition involves ventricles as well as atria, and the beat is going through an extra abnormal connection, also known as an accessory pathway (see image at right).- Wolff-Parkinson-White Syndrome (WPW) – In this condition, an extra electrical pathway between your heart's upper and lower chambers causes a rapid heartbeat. The extra pathway is present at birth and fairly rare. It usually isn’t life-threatening, but serious heart problems can occur. Treatment can stop or prevent episodes of fast heartbeats. Catheter ablation can permanently correct the heart rhythm problems.
Atrial Tachycardia
This rapid heartbeat accounts for 5-10% of tachycardia cases, originates in the heart’s atria. In this abnormal rhythm, a group of cells begins firing rapidly for no discernible reason.
Atrial Fibrillation (A-Fib)
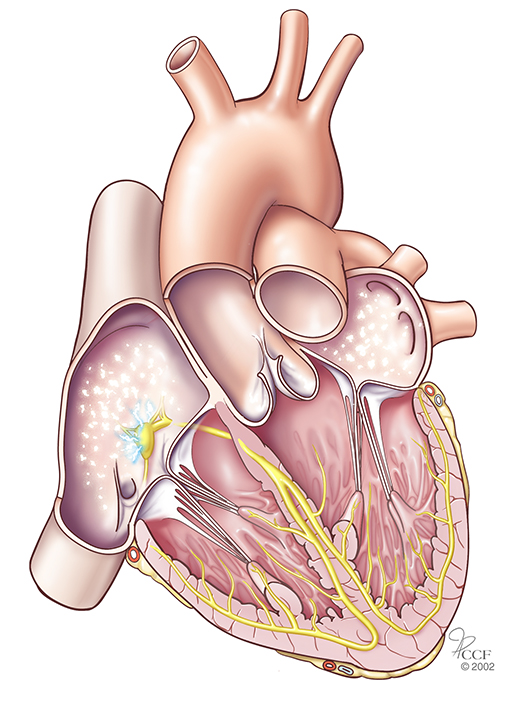 Of all the different types of arrhythmia, this is the term that most patients probably have heard of; that is almost certainly because this form of irregular heartbeat is so common. In fact, A-Fib is the most common type of arrhythmia in the world. In A-Fib, lots of electrical impulses begin and spread through the atria, all “competing” for a chance to travel through the AV node. This results in a rhythm that is irregular, rapid, disorganized, and chaotic – like an electrical storm in the atria – which leads to a loss of coordinated atrial contraction.
Of all the different types of arrhythmia, this is the term that most patients probably have heard of; that is almost certainly because this form of irregular heartbeat is so common. In fact, A-Fib is the most common type of arrhythmia in the world. In A-Fib, lots of electrical impulses begin and spread through the atria, all “competing” for a chance to travel through the AV node. This results in a rhythm that is irregular, rapid, disorganized, and chaotic – like an electrical storm in the atria – which leads to a loss of coordinated atrial contraction.
In A-Fib, the heart can beat up to 600 times in a minute in the atria, but the AV node only allows 200-250 of those beats through to the ventricle. In this situation, blood which is not being moved out of the atria can pool there, causing a clot and increasing the risk for a stroke. However, there are treatments available to mitigate this risk, from medications to stroke prevention devices, such as the Watchman device.
Atrial Flutter
This atrial arrhythmia is caused by one or more rapid circuits in the atrium. Atrial flutter is related to atrial fibrillation, but is usually more organized than A-Fib. While A-Fib can organize into atrial flutter and atrial flutter can disorganize into A-Fib, atrial flutter can be found as an independent entity as well. The most common atrial flutter pattern causes a short circuit around the tricuspid valve (the first valve that blood encounters when entering the heart, positioned between the right upper chamber and right lower chamber) Atrial flutter portends the same risk for stroke as A-Fib, and often needs similar types of treatment.
Bradycardia / Bradyarrhythmia
Bradycardia is a very slow heartbeat, less than 60 beats per minute, and it might be normal for some people. In trained athletes, for example, a low heart rate during exercise may be normal. However, when bradycardia is an abnormal state, we call it bradyarrhythmia and must address it with you through further testing and treatment.
Types of bradyarrhythmias include:
- Sinus Node Dysfunction – Sometimes, the heart rhythm can be slow due to abnormal sinus node (sinoatrial node, or SA node) impulse delivery, which can cause fatigue, shortness of breath, or exercise intolerance due to the inability of heart to keep up with your body’s needs. Also, the sinus node can experience pauses after the termination of A-fib or atrial flutter, which can result in syncope.
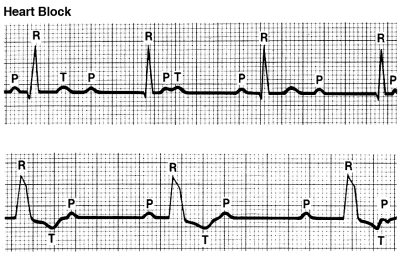 Heart Block – the electrical impulse is delayed or completely blocked as it travels from the SA node to the ventricles. The block or delay may occur in one of two places, each leading to a slow or irregular heartbeat, and each with different levels of severity:
Heart Block – the electrical impulse is delayed or completely blocked as it travels from the SA node to the ventricles. The block or delay may occur in one of two places, each leading to a slow or irregular heartbeat, and each with different levels of severity:- The His-Purkinje network (the intraventricular conduction system from the bundle of His to the distal Purkinje fibers, which carries the electrical impulses to the ventricles). This form of heart block can lead to complete heart block in over 50% of patients, and needs immediate treatment.
- The AV node – these heart blocks are usually more benign.
Ventricular Arrhythmias
These arrhythmias begin in the lower chambers (ventricles) of the heart, and can be life-threatening if not treated promptly. Variations include:
- Ventricular Fibrillation (V-fib) – In this condition, an erratic, disjointed firing of electrical impulses from the ventricles causes the ventricles to quiver, and they cannot produce an effective contraction. This means that they cannot deliver an adequate blood supply to the rest of the body
- Note: V-fib is a medical emergency that must be treated with defibrillation (delivering an energy shock to the heart muscle) as soon as possible to prevent death.
- Ventricular Tachycardia (V-tach) – As the name implies, this is a rapid heartbeat the originates in the ventricles. Because of the rapid heartbeat, the heart is unable to adequately fill with blood, so less blood is available to pump throughout the body.
V-tach is a serious condition and should be evaluated by a cardiologist at once. It is usually seen in patients who have previously had a myocardial infarction (MI, or heart attack) which has created a scar, which is “dead” tissue. The electrical signal goes around the scar, and this leads to a short circuit. However, a small proportion of patients can also have V-tach with a normal heart. In those patients, the condition doesn’t cause death, but can lead to syncope.
- Note: V-tach is a medical emergency that must be treated with defibrillation (delivering an energy shock to the heart muscle) as soon as possible to prevent death
Genetic Conditions With Risk of Ventricular Arrhythmias
These disorders are not common, but if someone in your family has experienced one, it’s best to be evaluated by a physician to confirm your own heart health status.
- Long QT Syndrome – The QT interval on the ECG represents the time it takes for the heart muscle to contract and then recover. When this interval is longer than normal, it increases the risk for a life-threatening form of ventricular tachycardia called “torsade de pointes.”
- Brugada Syndrome – This is an inherited sodium channel abnormality that can lead to irregular heartbeats in the heart's lower chambers and cause ventricular arrhythmia. If it’s not treated, the irregular heartbeats can cause fainting (syncope), seizures, difficulty breathing, or sudden death. These complications typically occur when an affected person is resting or asleep. Brugada syndrome usually becomes apparent in adulthood, although it can develop any time throughout life.
- Hypertrophic Cardiomyopathy (HCM) – This is a condition in which the myocardium (heart muscle) becomes hypertrophied (abnormally thick.) The thickened heart muscle can make it harder for the heart to pump blood, and trigger a ventricular arrhythmia. Hypertrophic cardiomyopathy often goes undiagnosed because many people with the disease have few, if any, symptoms and can lead normal lives with no significant problems. However, in a small number of people with HCM, the thickened heart muscle can cause shortness of breath, chest pain or problems in the heart's electrical system, resulting in life-threatening abnormal heart rhythms (arrhythmias).
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) – ARVC is a disorder which causes part of the myocardium to break down over time, increasing the risk of an arrhythmia and sudden death. This is a form of heart disease that usually appears in adulthood, and may not cause any symptoms in its early stages. However, affected individuals may still be at risk of sudden death, especially during strenuous exercise. When symptoms occur, they most commonly include a sensation of fluttering or pounding in the chest (palpitations), light-headedness, and fainting (syncope). Over time, ARVC can also cause shortness of breath and abnormal swelling in the legs or abdomen. If the myocardium becomes severely damaged in the later stages of the disease, it can lead to heart failure.
- Idiopathic Ventricular Fibrillation – This condition is a rare cause of sudden cardiac arrest (SCA) or sudden cardiac death (SCD.) Patients who have IVF present with a sudden onset of ventricular fibrillation (V-fib) of unknown origin that is not identified even after extensive diagnostic testing. The exact incidence of IVF is unknown, but fortunately, it’s declining with the advance of diagnostic testing and the discovery of primary arrhythmia syndromes, such as the Brugada syndrome and long-QT syndrome.