Heart failure (HF) affects approximately 5.7 million adults in the United States according to the Centers for Disease Control and Prevention. If not properly managed, HF can lead to frequent hospitalizations. A heart failure hospitalization should be viewed as a sentinel event. Five year survival after a heart failure hospitalization is only 20 percent, a prognosis that is worse than most cancer diagnoses. Importantly, if HF is properly managed by team of skilled heart failure clinicians, prognosis and quality of life can improve.
According to the American Heart Association (AHA), the most common symptoms of HF include:
- Shortness of breath (dyspnea)
- Persistent coughing or wheezing
- Buildup of excess fluid in body tissues (edema)
- Fatigue
- Lack of appetite, nausea
- Confusion, impaired thinking
- Increased heart rate
It is important for patients to be knowledgeable about heart failure symptoms. Alerting your health care team to subtle changes in symptoms can prevent a heart failure hospitalization and allow you to live a full and productive life. Signs and symptoms to monitor are:
- Weight gain of > 3 lbs in 1 day or 5 lbs in 1 week
- Swelling in ankles or other parts of the body
- Difficulty breathing
- Difficulty performing activities of daily living due to shortness of breath or fatigue
- Feeling like one has "the flu"
- Lightheadedness or dizziness
- Chest pain
There are many effective treatments for patients with heart failure. Below are common medications used to help strengthen weakened hearts and/or manage symptoms of congestion.
- Angiotensin Converting Enzyme (ACE) Inhibitor
- Angiotensin Receptor Blocker (ARB)
- Angiotensin-Receptor Neprilysin Inhibitor (ARNI)
- Diuretic
- Beta-Blocker Digoxin
- Imdur/hydralazine
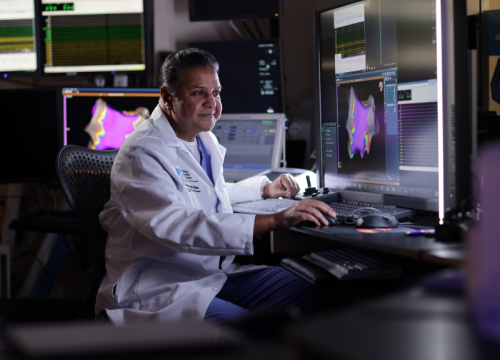
In patients with weakened hearts, implantable cardioverter-defibrillators (ICD), cardiac resynchronization therapy (CRT), left ventricular assist devices (LVAD), or heart transplantation may be explored. Percutaneous coronary intervention (PCI) (also referred to as angioplasty) or coronary artery bypass may be recommended for heart failure caused by coronary artery disease. For heart failure caused by valvular disease, valve replacement may be recommended.
To help prevent future hospitalizations, the National Heart, Lung and Blood Institute recommends:
- Taking all prescribed medications correctly and reporting any medication issues to patient’s doctor and/or pharmacist right away
- Making sure to follow the correct diet (for example, avoiding salty foods)
- Avoiding alcohol
- Minimizing the risk of respiratory infections such as the flu and pneumonia through vaccinations
The Valley Hospital Heart Failure Program treats and manages heart failure patients in an outpatient setting on the hospital’s main campus. The program, which is certified by The Joint Commission, takes a multidisciplinary approach to care. The team works closely with pharmacy and palliative care staff. There is a strong focus on patient training and education to empower patients to effectively manage their conditions. For more information on the program, please call 201-447-8018.