EXEMPLARY PROFESSIONAL PRACTICE focuses on how nurses throughout the organization are involved in shared governance and shared decision-making, and explores how interprofessional collaboration promotes quality excellence in a culture of safety.
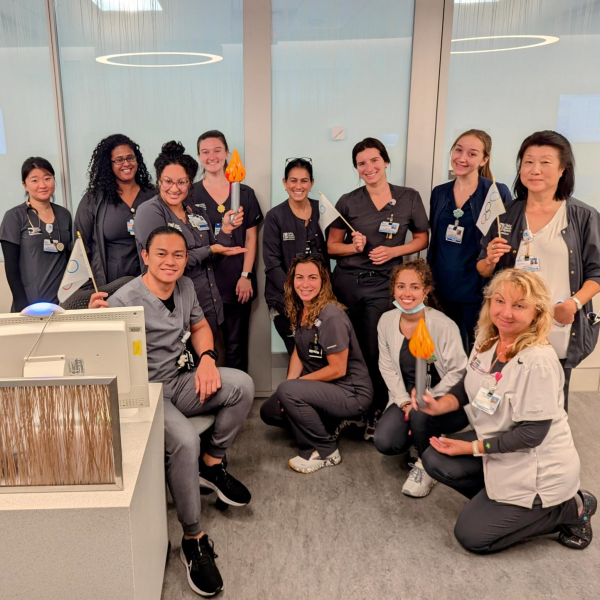
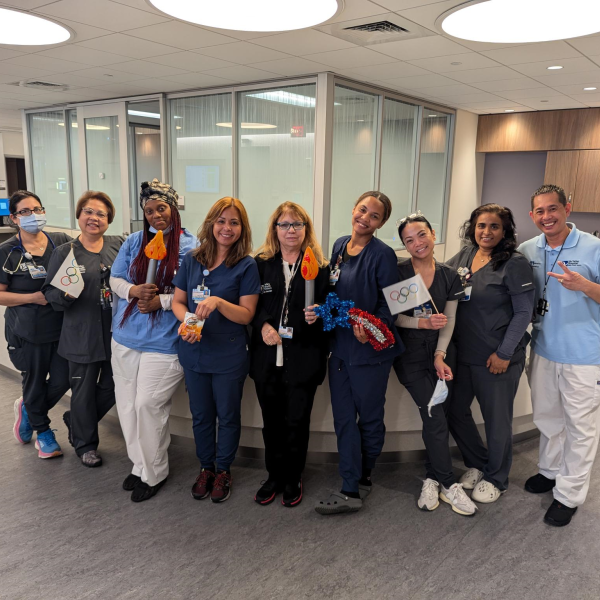
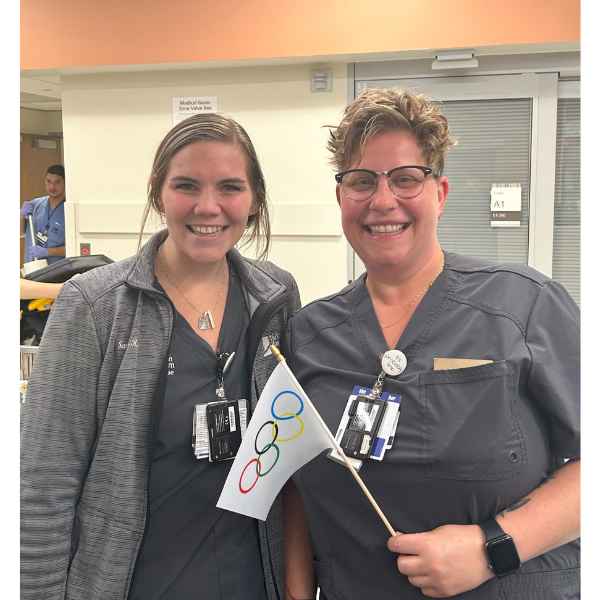
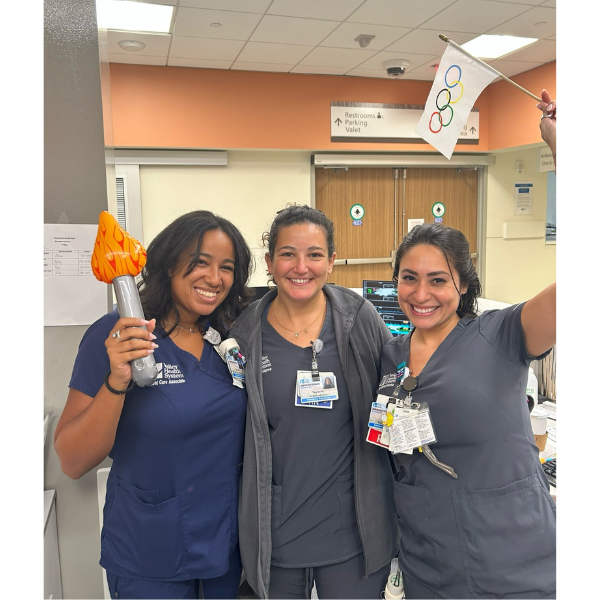
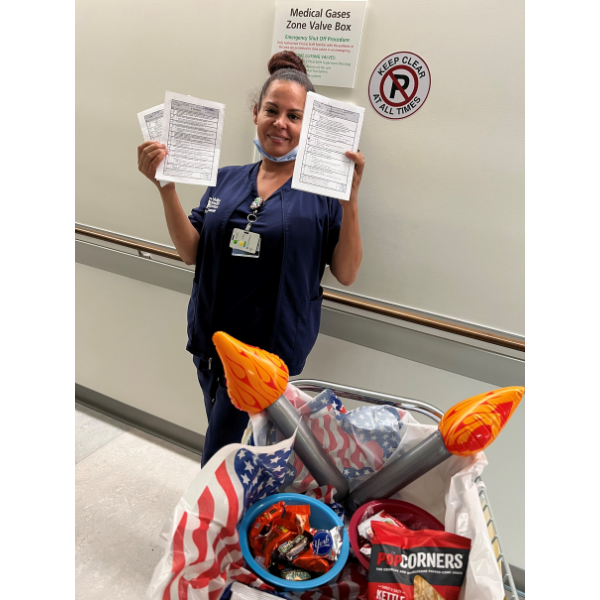
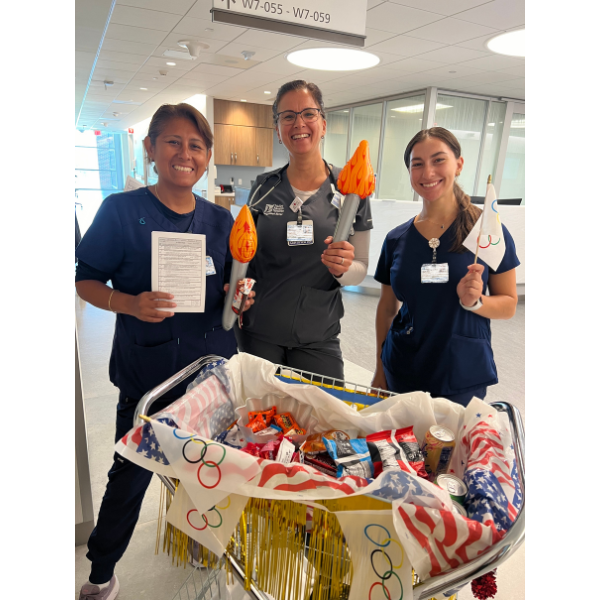
Valley Hosts the Quality Olympics!
Last summer, Valley hosted the Quality Olympics to help us increase compliance with our quality measures, boost staff engagement and celebrate our successes in a fun, creative way!
Launched by Valley’s Quality and Performance Improvement (QPI) team, the Quality Olympics focused on completing preventive measures for four critical hospital-acquired conditions: catheter-associated urinary tract infection (CAUTI), central line-associated bloodstream infection (CLABSI), hospital-acquired pressure injury (HAPI), and falls.
Over four weeks, nurses and patient care associates (PCAs) from The Valley Hospital’s Emergency Department, medical-surgical units, and critical care units used Kamishibai cards, or K-cards, for each of the four hospital-acquired conditions. The K-cards included reliability criteria, or proactive measures to follow to help prevent the condition. Those who completed all of the criteria earned a gold K-card!
To keep up the momentum and excitement, every week, the top three units that earned the most gold K-cards were announced. By the end of the contest, an incredible 520 K-cards were completed! The top nurse and PCA from each unit were recognized in a closing ceremony and were presented with an Olympic medal and gift card.
Congratulations to all of the nurses and PCAs involved for your hard work, dedication, and unwavering commitment to providing safe, reliable care!
Valley Presents at National Conference on NICU Developmental Care Team
In March 2024, Monika Reisenauer, DNP, APRN, NNP-BC, Lead Advanced Practice Provider, Inpatient and Outpatient Pediatrics, and a team of six Neonatal Intensive Care Unit (NICU) clinicians and staff attended the annual Gravens Conference on the Environment of Care for High-Risk Newborns to present on the development and impact of Valley’s Neonatal Developmental Care Team.
For the presentation, Valley’s team discussed how the NICU environment – specifically sound, lighting, and temperature – can impact the development of preterm infants, as well as the importance of therapeutic touch, supportive positioning, and parent/family involvement in care. As a result of the team’s efforts, Valley has seen a decrease in the length of stay for NICU infants, as well as improved Infant Positioning Assessment Tool (IPAT) and Bayley Scales of Infant and Toddler Development (BSID) scores.
Valley’s Neonatal Developmental Care Team is dedicated to fostering an environment within the NICU that maximizes neurodevelopmental progression of every infant. The team strives to nurture infant/parent relationships and is committed to coordinating family-centered care within the NICU to have a positive impact on life-long neuro-developmental outcomes.

Valley Medical Group Launches Nurse-Led Trimester Education Classes
 As part of her role as an OB/GYN nurse, Mindy Lugo, MSN, RN, VMG Midwifery and OB/GYN Paramus 140, was providing pregnancy education to her patients during their visits but saw an opportunity to teach this information in a broader, more universal way. As a result of her efforts, in 2024, Valley Medical Group’s trimester education classes were launched!
As part of her role as an OB/GYN nurse, Mindy Lugo, MSN, RN, VMG Midwifery and OB/GYN Paramus 140, was providing pregnancy education to her patients during their visits but saw an opportunity to teach this information in a broader, more universal way. As a result of her efforts, in 2024, Valley Medical Group’s trimester education classes were launched!
Mindy began by teaching a third trimester education class for pregnant patients and, soon after, the program expanded to also include first and second trimester classes with support from Colleen DiBiase, BSN, RN, VMG OB/GYN Ramsey and Wayne, and Theresa Marciano, BSN, RN-BC, HN-BC, VMG OB/GYN Fair Lawn and Montvale. Together, Mindy and Colleen teach the trimester-specific classes, and Theresa handles the logistics of the program, including marketing, sign-ups, and ensuring each class includes the most up-to-date information.
Valley Medical Group’s trimester education classes are free of charge and open to the entire community. Classes are held virtually every month and feature important pregnancy-related health topics, as well as Valley-specific information such as how to use the patient portal for communication and results, and details of the visitor policy for when patients deliver. Each class ends with ample time for a question-and-answer session.
The class schedule and link to register are listed on Valley’s website to help patients plan ahead. Those who register are also sent a pre-survey link to submit any specific topics they would like to hear about in the class. This helps Mindy, Colleen, and Theresa ensure they are capturing input from patients and adjusting the classes to fit their needs.
In addition to the wealth of information patients receive through the trimester education classes, they are also encouraged to explore Valley’s Center for Family Education and Thrive! programs to ensure they are taking advantage of all of the wonderful education opportunities that Valley offers.
Lactation and Outpatient Rehab Departments Partner to Treat Patients with Clogged Milk Ducts
In 2023, Justine Ward, PT, DPT, WCS, CBBA, Board-Certified Clinical Specialist in Pelvic Health Physical Therapy, Outpatient Rehabilitation, approached Valley’s Lactation Department with an innovative, new treatment option for patients who experience clogged milk ducts: the use of therapeutic breast ultrasound.
Justine, who is also certified in breast milk duct ultrasound therapy, had performed a case study where her team was able to successfully treat a patient with a clogged milk duct by using ultrasound therapy, soft tissue mobilization, and education regarding self-care techniques for home. After presenting her findings at an OB Grand Rounds meeting for Valley Medical Group and community OB/GYNs, Justine and Katie Ver Hage, MSN, BSN, RNC-OB, C-EFM, IBCLC, Manager of Maternal-Fetal Medicine, Family Education and Lactation, began taking steps to offer this service to all patients starting in 2024.
When a breastfeeding patient comes to Lactation with a clogged milk duct, the patient is guided on how to unclog it. If those efforts are not successful, the patient is directed to obtain a referral from their OB/GYN or pediatrician to see Outpatient Rehab. Through this partnership and well-established communication between the two departments, in many instances, patients are able to receive same-day services. Patients then return to Lactation for follow-up.
As a result of this collaboration, last year, 18 patients were successfully treated for clogged milk ducts in Outpatient Rehab using ultrasound therapy. We look forward to continuing to raise awareness about this innovative treatment option to provide the best care to our patients.
Move 2 Improve Taskforce Develops Nurse-Led Mobility Guidelines

In our continuing efforts to improve patient mobility rates, last year, Valley’s Move 2 Improve taskforce came together to develop nurse-led mobility guidelines.
The interdisciplinary taskforce, with nursing, physician, and physical therapy representation, created the guidelines based on a patient’s Bedside Mobility Assessment Tool (BMAT) level. Each BMAT level has associated overall goals, nursing activity recommendations, out-of-bed to chair goals, and equipment options for mobility and fall prevention.
In December 2024, three nurses – Jessica Zingaro, BSN, RN, MedSurg-BC; Carrie Kral, BSN, RN, and Tony Vijayan, BSN, RN – and three patient care associates (PCAs) – Hanane Elyadini, Iwona Draheim, and Karina Parra – participated in a Test of Change using these new guidelines on Valley’s West 5A Bariatric/Surgical unit. Working together, each nurse-PCA pair was able to improve mobility rates each day that they implemented the guidelines. As a result, the overall mobility rate on the unit increased by five percent during that time frame. Due to the success of the pilot, all inpatient nurses and PCAs will be trained on how to use the new mobility guidelines in 2025.
In addition to the development of the nurse-led mobility guidelines, last year, the Move 2 Improve taskforce also refined our Meditech documentation to better reflect mobility activities and expanded the mobility rounder technician (MRT) role to two additional inpatient units.
Valley Home Care’s Nursing and Rehabilitation Teams Establish Pods
In 2024, Valley Home Care’s (VHC) nursing and rehabilitation teams formed pods to enhance communication, efficiency, and outcomes for patient care.
There are five pods in total, representing each of the four VHC nursing teams and the specialty care team. Each pod includes a nurse, case manager, and physical, occupational, and/or speech therapist. Once or twice a week, the teams meet virtually to discuss their mutual patients, how they are progressing in their treatment, and next steps for care. This allows all members of the care team to be in alignment to ensure their patients receive the safest, most efficient care and, in turn, improve outcomes.
As a result of this collaboration, from January 2024 through January 2025, several of VHC’s Outcome and Assessment Information Set (OASIS) quality measures improved as follows:
- 20% Improvement in Discharge Function Score
Evaluates the functional status of patients at discharge and assesses their ability to perform daily self-care and mobility activities - 20% Improvement in Total Normalized Composite: Change in Mobility
Assesses the improvement of a patient's mobility from the start of care through discharge - 22% Improvement in Total Normalized Composite: Change in Self-Care
Assesses the improvement of a patient’s ability to perform self-care activities from the start of care through discharge
Valley Home Care, Hospice and Rehab Collaborate to Create Referral Workflow
To standardize the referral and scheduling process across Valley Home Care (VHC), Hospice and Rehabilitation, a multidisciplinary team came together last year to create a more efficient workflow process.
Representatives from each of the three areas, as well as employees from Quality and Performance Improvement, Case Management, and Finance, first completed an entire mapping of all of the standard operating procedures (SOP) to identify any gaps in care. From there, the team created new processes together to improve workflow efficiencies and ensure patients were receiving the safest next level of care.
Some of the team’s interventions include:
- Educating providers on the new referral process
- Creating new SOPs for hospice infusions and hospice-to-hospice transfers
- Standardizing scripting for no-answer calls
- Ensuring communications from insurance specialists are clear and easy for patients to understand
This is just one of many ways that interprofessional collaboration has helped us to provide safe, reliable, high-quality care to our patients and their families.
VHC Nursing Teams Implement Daily Stand-Up Meetings
To help foster improved communication, increased efficiency, and enhanced patient care, last year, Valley Home Care’s (VHC) nursing teams implemented a daily stand-up meeting.
Every morning at 8:30 a.m., VHC’s nurse managers conduct a quick virtual meeting with their team members to review everyone’s schedule for the day, see if anyone needs assistance with their caseload, and discuss any concerns they may have. Managers also remind the nurses of any pertinent information and deadlines coming up, such as annual competencies, requirements from Employee Health, and staff events.
Since implementing the daily stand-up meetings, VHC’s nursing leadership team has received positive feedback on how it has helped nurses anticipate and prioritize the needs of their patients for the day.
“I find that since starting the morning meetings, my day flows a lot smoother. There are fewer phone calls and emails throughout the day, allowing us to focus on patient care. We are able to address concerns and discuss patients in real time. We also have the pleasure of seeing our teammates daily!” – Kaitlin Ryan, RN, Nursing Team 4
Advanced Practice Nurses Join Valley’s Radiation Oncology and Infusion Teams
Last year, Valley was proud to welcome two advanced practice nurses (APNs) to the Valley-Mount Sinai Comprehensive Cancer Care team: Kelly LoPresti, APN, Radiation Oncology, and Alexa Segna, APN-BC, AOCNP, Infusion.
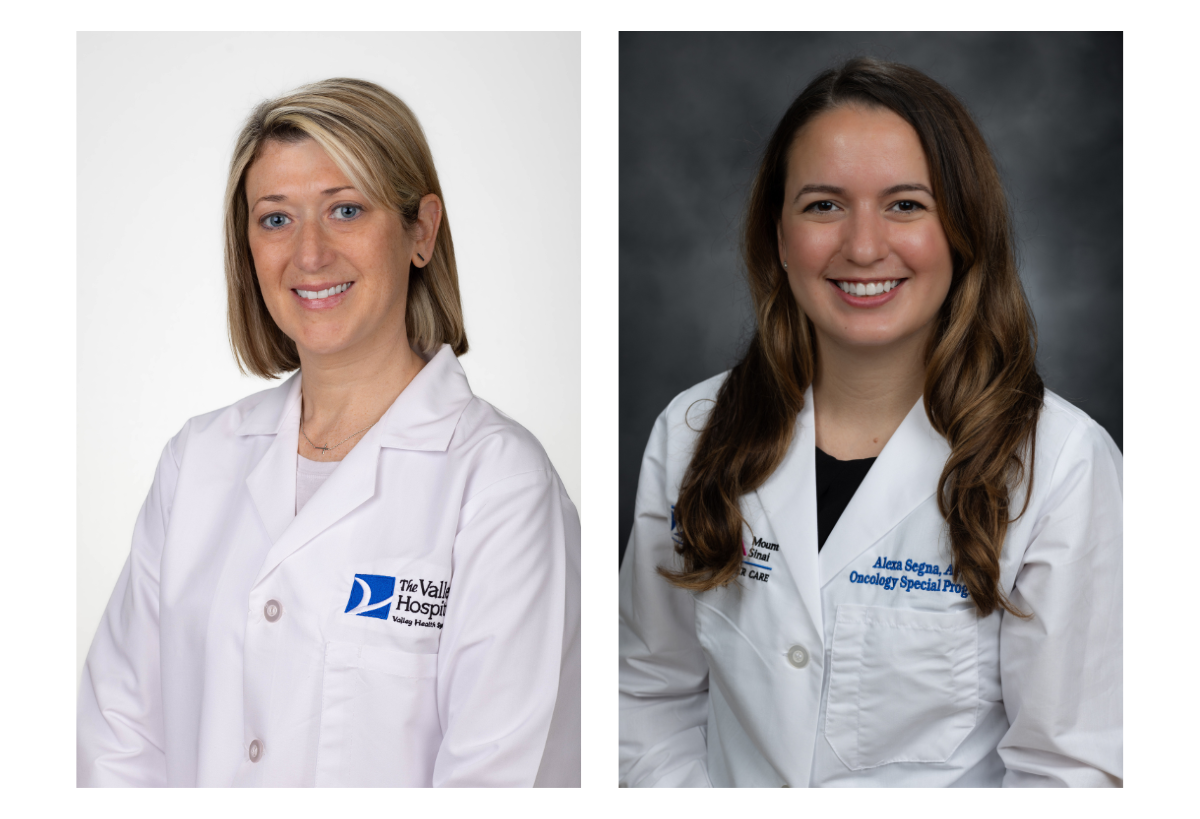
Kelly LoPresti, previously a nurse navigator with Valley’s Gamma Knife Center for more than 10 years, pursued an advanced degree as a nurse practitioner and, in February 2024, joined the Radiation Oncology team as their first APN. Through her new role, Kelly provides comprehensive care for patients undergoing radiation therapy, from initial consultation through survivorship, along with streamlining and expediting care for inpatients requiring treatment. She has a primary focus on prostate cancer, collaborating with the Urologic Oncology multidisciplinary team. Kelly also remains active in the Gamma Knife Center, collaborating with Valley’s neurosurgery team on malignant and benign intracranial conditions.
Alexa Segna joined in July 2024 as Valley’s first Infusion-dedicated advanced practice provider (APP). As part of her role, she provides symptom management, urgent evaluation, and care onsite at the Luckow Ambulatory Infusion Center. If a patient receiving infusion therapy has a reaction or issue, Alexa offers an additional layer of support to the nursing team. The goal of this program is to maintain patients in the appropriate setting when receiving their cancer care and to reduce emergency room utilization and inpatient admissions. Patients are sent to the hospital as required by their acuity level and condition. Valley is currently recruiting for a second Infusion-dedicated APP to ensure on-site provider coverage seven days a week.
With the addition of APPs to our care teams, Valley is able to provide safe, high-quality care to our patients and their families, while also improving access to care and enhancing outcomes.
2024 Highlights from VMG’s Nurse Practice Council
Valley Medical Group’s Nurse Practice Council had a busy year! In 2024, council members focused on using evidence-based research and literature searches to address issues and develop solutions.
Below are a few highlights from last year:
- As a result of a high number of sharps injuries occurring in VMG practices, council members researched and recommended a safer needle for employees to use and worked to replace this as a supply item for practices to order.
- Through group discussion, members have been able to create and improve documentation and charting efficiency in Athena, VMG’s electronic medical record, resulting in positive impacts on workflow.
- The group provided feedback on the new, robust competencies developed by Valley’s Education Department.
- The Council is beginning research on how to improve breast cancer screening compliance.
The mission of VMG’s Nurse Practice Council is to set, implement, and maintain a nursing clinical practice standard in outpatient areas, according to evidence-based practice, research findings, and/or regulatory agency requirements. Chaired by Colette Kramer, MA, RN, CPNP-PC, Clinical Educator, VMG Quality, and with nurse representatives from multiple specialties, the group meets bimonthly to discuss topics related to practice excellence, professional development, quality and safety, informatics, and communication.

Valley APN Leads Comprehensive Training on New Cancer Treatment
Last year, Laura LoPresti, MSN, AGNP-C, OCN, Advanced Practice Nurse, West 6A Oncology, developed and implemented a comprehensive education plan on a new treatment option for multiple myeloma: bispecific T-cell engagers (BiTEs) immunotherapy.
BiTEs are a type of immunotherapy designed to help the immune system find and destroy cancer cells. While it has been shown to be very effective in treating multiple myeloma, there are two potentially life-threatening complications that can occur: Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS). Education is key for close monitoring and early detection of these serious side effects, as they are highly treatable in their early stages.
Laura led the charge in developing an education plan to train Valley’s Rapid Response Team nurses, inpatient and outpatient oncology nurses, Emergency Department nurses, the critical care team, the respiratory care team, and providers on how to both administer the therapy and monitor for complications. The plan included a mandatory online education course, as well as a simulation video on different scenarios that clinicians can encounter during patient treatment.
As a result of Laura’s hard work to provide extensive training to all involved physicians, nurses, and staff, Valley successfully treated its first patient with BiTEs immunotherapy in January 2025!