The Valley Hospital is now open at 4 Valley Health Plaza in Paramus. (You may need to use 650 Winters Avenue for GPS.) All emergency care is now being provided at this location. Emergency care is no longer available at our Ridgewood campus.
Virtual Fertility Appointments Available
The Valley Hospital Fertility Center is seeing patients virtually for consultations and follow-up visits (in cases where a physical examination is not required). Call 201-634-5400 to schedule a virtual visit.
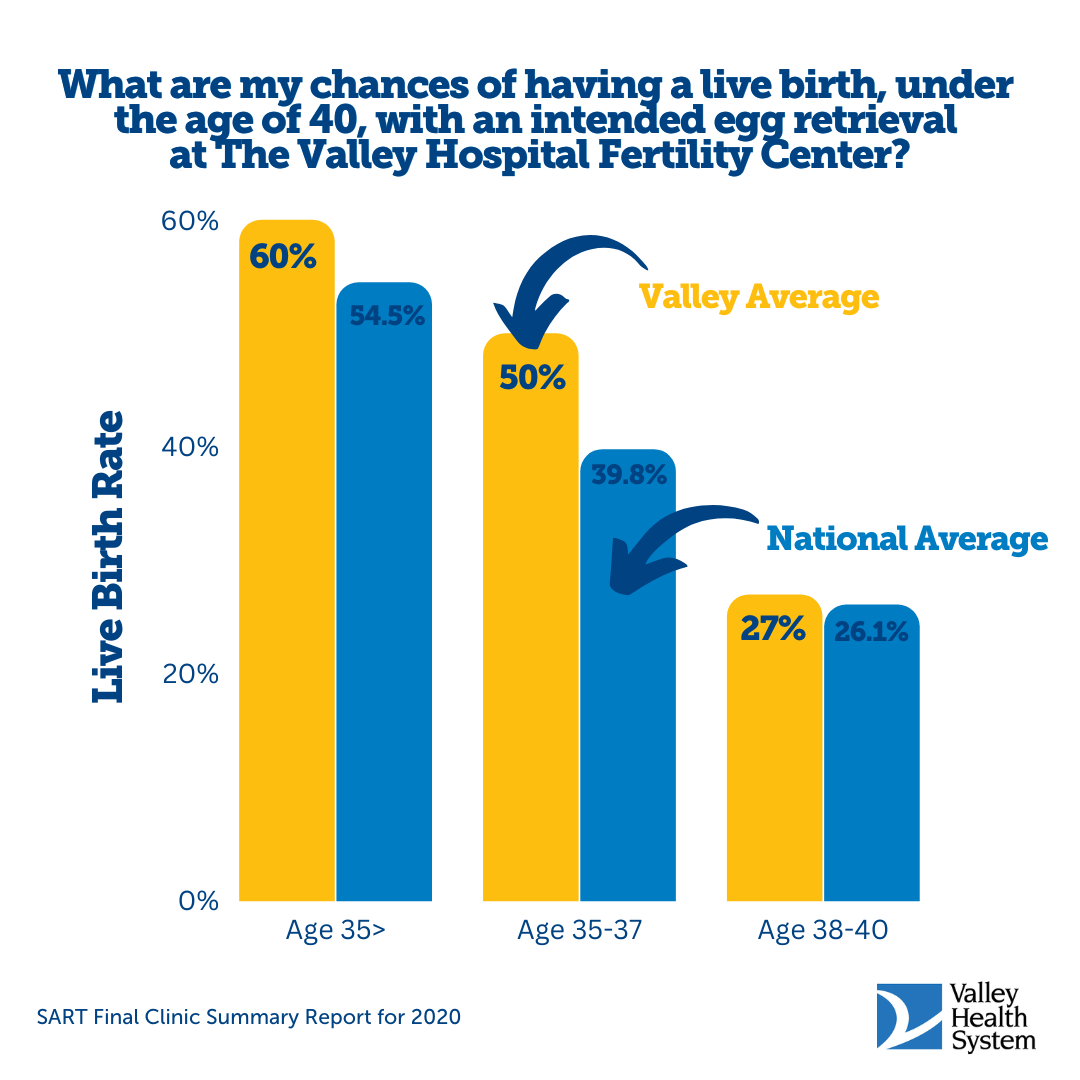
Outcomes at The Valley Hospital Fertility Center
We know that the most important measure of success for you is a successful pregnancy resulting in a baby.
At the Valley Hospital Fertility Center, we’re happy to report that on that measure, we deliver. Our in vitro fertilization (IVF) success rates per frozen cycle are higher than the national average for all age groups — from under 35 to over 42.
For the latest results available for IVF cycles performed at Valley, please visit the Society for Assisted Reproductive Technology (SART)’s Valley clinic summary report.
Patrice and Yolanda's Story

When Patrice and Yolanda started thinking about their road to family, they came across The Valley Hospital Fertility Center. After a six-year fertility journey, they welcomed their daughter, Judah, into the world.
SART Data
SART Final National Summary Report for 2020
The Valley Hospital Fertility Center Final Clinic Summary Report for 2020
The Valley Approach to Fertility Care
We understand the emotional and psychological concerns of couples seeking infertility treatment.
Our reproductive endocrinologists and nurses possess not only the medical expertise responsible for superior success rates, but the caring and compassion that leads many patients to recommend our program to family members and friends.
Our Areas of Care
Fertility Assessment
Valley offers comprehensive fertility assessment for men and women to identify any infertility issues.
Infertility Treatment
Valley offers the full range of basic and advanced infertility treatment options.
- IVF (In Vitro Fertilization)
- IUI (Intrauterine Insemination)
- Ovulation Induction
- Gestational Surrogacy
- Donor Egg Services
Fertility Preservation
Valley offers oncofertility options for individuals undergoing cancer treatments.
- Egg Freezing
- Embryo Freezing
Genetic Screening
We provide genetic screening of embryos prior to implantation.
- Preimplantation genetic testing (PGT)
LGBTQ Family Building
We welcome all LGBTQ individuals and couples for family building.
Conditions Treated
- Infertility
- PCOS (polycystic ovary syndrome)
- PCOD (polycystic ovary disease)
- Endometriosis